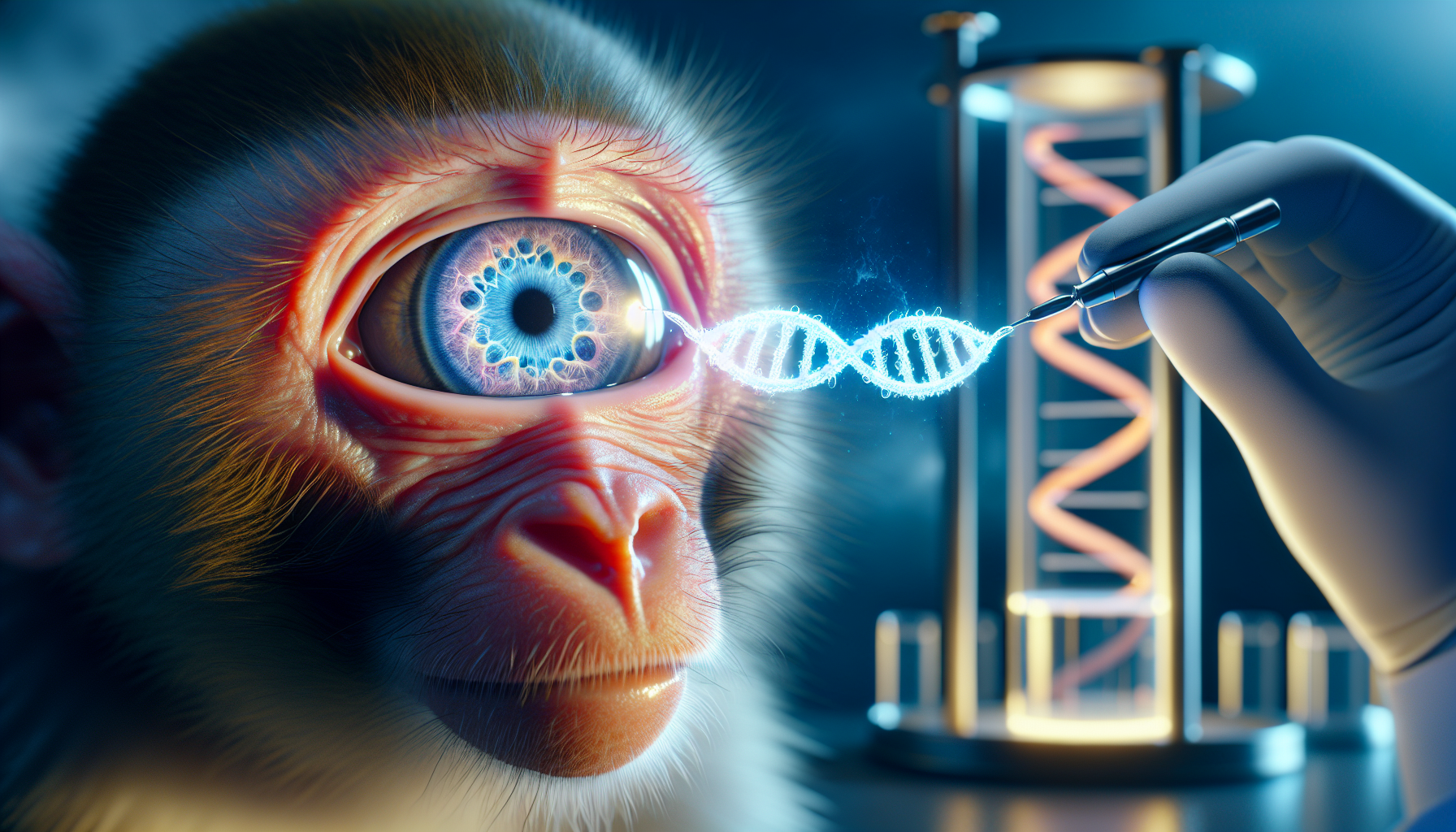
In a significant stride forward for eye care, a study reveals that human stem cell transplants have been successfully used to repair macular holes in a primate model. This breakthrough research was published in the scientific journal, Stem Cell Reports, on October 3rd. Post-transplantation, it was observed that the macular holes were fully remedied through the continuous growth of retinal tissue in the affected area.
As per Michiko Mandai, the leading researcher from Kobe City Eye Hospital, this is the first confirmation of embryonic stem-derived retinal organoid sheet transplantation facilitating macular hole closure in a non-human primate model. The findings imply that this technique could potentially offer a practical, safe, and effective treatment for even the most challenging macular hole cases, with minimal risks involved.
Macular holes are tiny gaps that appear in the macula, the central part of the eye’s retina. These holes can distort or blur central vision, making it challenging to read, drive, or see intricate details. Even though surgical advancements in the past decade have resulted in closure rates surpassing 90%, persistent and recurrent cases post-surgery continue to be problematic. Cell-based therapy is envisaged as a promising strategy for restoring visual function in cases of retinal degenerative diseases. While retinal transplantation has demonstrated successful anatomical results, improvements in visual function are limited, and peripheral visual field defects are unavoidable.
In this study, Mandai and her team explored the potential of overcoming these obstacles by transplanting human embryonic stem cell-derived retinal organoid sheets. The transplantation process resulted in successful graft survival, maturation, and the growth of light-detecting retinal cells, known as photoreceptors, including rods and cones. Furthermore, the experiments showed enhancements in eye fixation and light response.
However, the researchers highlighted certain limitations, such as mild transplantation rejection, which was managed with steroid injections. Mandai stated that this mild rejection might have restricted the functional integration of the transplanted tissue. Moreover, this was a single-case result for one eye, and the primate model did not exactly replicate the human refractory macular hole pathology. Despite these limitations, the findings suggest that the surgical technique could be applicable for human macular holes.
The researchers are of the opinion that more studies are necessary to validate the benefits of the stem cell-derived retina, including its protective effect on host retinal cells. Further research is also needed to comprehend how cell composition in the graft impacts visual function. Going forward, the research team intends to investigate whether some form of synaptic communication can be established between the host and graft during a longer observation period.

Comments are closed for this post.