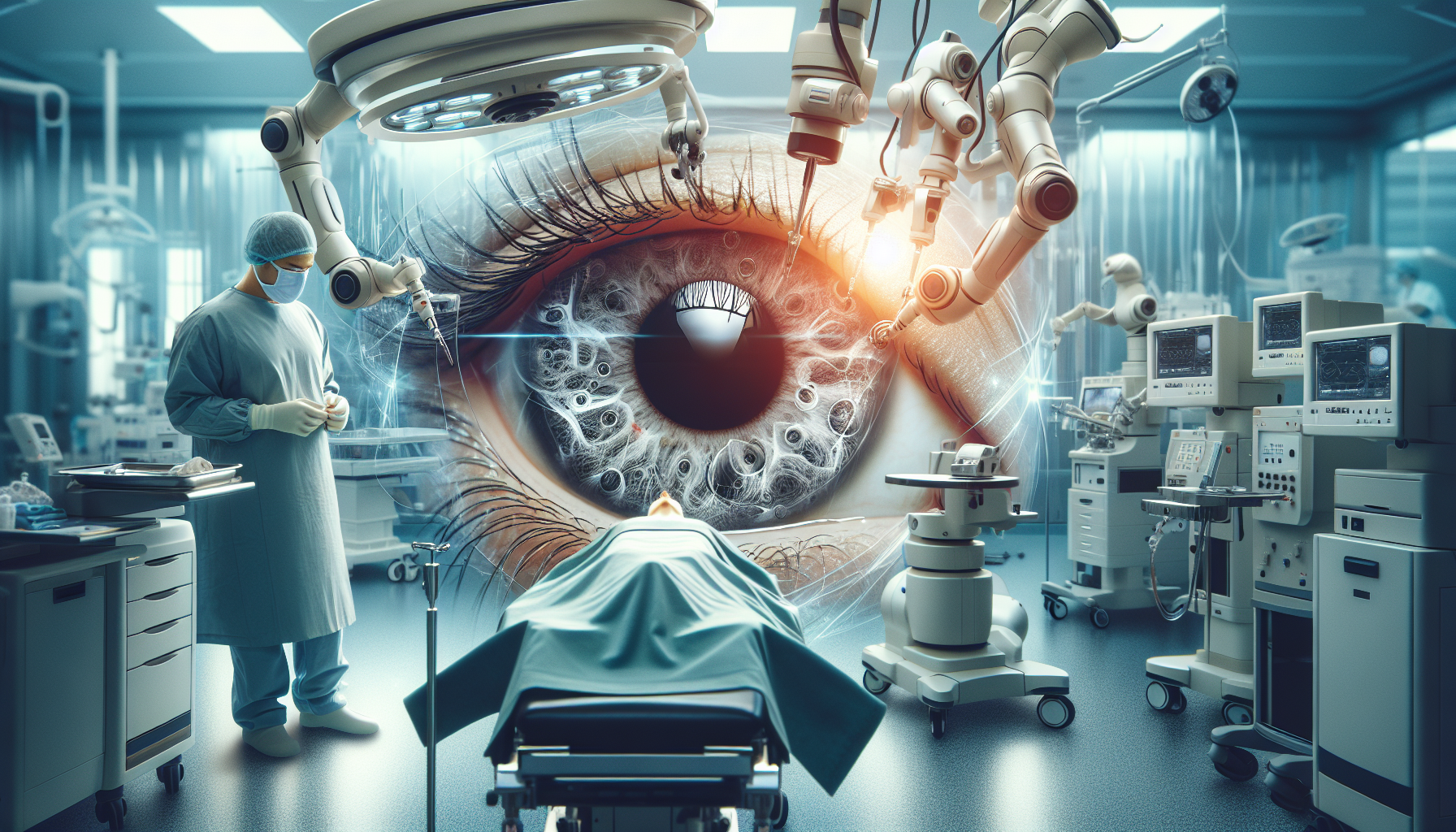
Retinal surgery, one of the most intricate procedures within the medical field, involves working with a layer of cells less than a millimeter thick. This delicate operation requires surgeons to navigate through challenges such as the patient’s eye movements, breathing, and even their own hand tremors. However, a recent collaborative innovation from the University of Utah’s John A. Moran Eye Center and John and Marcia Price College of Engineering might just revolutionize this process.
This innovation is a state-of-the-art robotic surgery device designed to provide surgeons with unprecedented precision. The robot, capable of executing movements as minuscule as 1 micrometer (smaller than a human cell), is mounted directly on the patient’s head. This configuration allows it to compensate for any subtle or significant head movements, keeping the eye stable from the robot’s perspective. Furthermore, the robot minimizes the surgeon’s movements to suit the tiny surgical site inside the eye, counteracting any hand tremors in the process.
This groundbreaking device is still undergoing testing but has promising potential to enhance patient outcomes and support cutting-edge treatments like gene therapies for inherited retinal diseases. Initial testing on enucleated pig eyes has proven successful, as documented by Jake Abbott, a professor in the U’s Department of Mechanical Engineering, and Moran Eye Center retinal specialist Paul S. Bernstein in the journal Science Robotics.
Inherent in the retina are light-sensitive rod and cone cells that are fundamental to vision. Certain inherited disorders can disrupt these cells, resulting in various degrees of vision impairment. However, new gene therapy techniques could potentially reverse these conditions. “The field of vision treatments is evolving rapidly. Our aim is to equip surgeons with improved capabilities to keep pace with this advancement,” Abbott said.
The U.S. Food and Drug Administration’s first approved gene therapy for an inherited retinal disease involves an injection into the space between the retina and the retinal pigment epithelium, another thin layer of cells. This microscopic target area introduces added complexity to the procedure, as the surgeon must inject the drug between two submillimeter-thin cell layers.
The researchers tested the robot’s performance using a unique method. A human volunteer, wearing special goggles, had an animal eye mounted just in front of their own. This setup let the researchers assess the robot’s proficiency in compensating for head motion and correcting hand tremors, all while operating on animal tissue, eliminating any risk to the volunteer.
The study reveals that the surgeons achieved higher success rates with the robotic device, performing subretinal injections while also averting ophthalmic complications. Moran Eye Center retinal surgeon and co-author, Eileen Hwang, believes the robot could enhance patient care. She stated, “The robot’s unique head-mounting feature could enable patients to receive subretinal injections under intravenous (IV) sedation instead of general anesthesia, leading to quicker recovery and increased safety for some patients. Robots could also deliver gene therapy medication more accurately than manual injections, resulting in safer, more consistent treatments.”
As this revolutionary robot transitions from the lab to the operating room, the interdisciplinary collaborations that conceived it continue to support its journey. “These collaborations at the University of Utah are truly remarkable,” Bernstein added. “Whenever I have ideas, I know that the engineers, chemists, and physicists are just a few blocks away.
Comments are closed for this post.